NOTE:
- The following E-log aims at discussing our patient de-identified health data shared after taking the guardian's signed consent.
- Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve the patients clinical problem with current best evidence based input.
- This E-log also reflects my patient's centered online learning portfolio.
I have been given this case to solve in an attempt to understand the topic of "Patient Clinical Data Analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and providing treatment best to our skills and wisdom.
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitted.
A 48 years old male , bus driver by occupation presented to opd with chief complains of huge abdominal distension.
CHIEF COMPLAINTS
➤Abdomen distension since 4months
➤Swelling of both legs since 2 months
➤Decreased urine since 1 month
DAILY ROUTINE
He used to get up by 5 and by 5:30 after getting freshed up he makes green tea for himself as he doesn't want to disturb his wife. After taking tea with couple of biscuits and a beetel nut, he goes to bus stand where he was working as a bus driver. Interestingly he starts from his home by 6 and covers 5km within 15mins.
By 6:30 he starts from siliguri for tinsukia which is around 1000kms.
At 9o clock he haunts his bus for breakfast where he takes rice dal with two pieces of fish and starts again.
His next stop was at 1 pm when he takes rice daal few pieces of small fish. And this time Instead of driving he takes rest and his assistant drives till 5pm.
Where bus stops and he takes a cup of milk with a packet of biscuit and beetel nut and starts his journey on driving seat.
He takes next hault at 10pm where he stops for dinner and again takes rice dal and fish and drives whole night and stops next day at 6am. He gets freshed up takes a cup of tea with biscuits and few betel nuts. And after taking rice daily fish in breakfast he finally reaches tinsukia In afternoon. After taking proper sound sleep till evening , he goes to a hotel where he takes 600ml of Desi beer with fishes. And sleeps by 10pm. He gets up by 5 next day and drove bus back to siliguri.
He takes this round trip two times in a week.
He used to smoke bidi and guthka amid his journey but never took alcohol cause of strict police screening.
He is into this profession since 28 years and took last trip 3 days before coming here so probably his last alcohol intake was then. Although he denied taking alcohol since few months.
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 4months ago. Following his daily routine he was cycling to earn his bread at around 6am. Few of his friends noticed that he is getting fat and obese but cause of his healthy life style he didn't pay much heed. Within 2-3 weeks few more people noticed that he is getting protruded abdomen which doesn't seems to fit in the puzzle according to his general physique. Some said that he has jaundice and sent him to a quack who seems to cure jaundice Within couple of hours. Although his so called jaundice didn't get cure but that quack said him that he got water in his belly and need to take proper medical care. And after few investigations he presented to our hospital with chief complaints of distended abdomen which is insidious in onset gradually progressive associated with decreased appetite since then.
Bilateral pedal edema extending upto knee since 2 months , pitting type increased on walking and relieved with rest
Decreased urinary output since 1 month
No h/o fever, cough, breathlessness.
No h/o drowsiness, loss of consciousness, palpitations, orthopnoea,pnd ,abdominal pain, fever,nausea vomiting.
PAST HISTORY :
No H/O similar complaints in past.
No H/O DM HTN TB asthma epilepsy CVA CAD.
PERSONAL HISTORY :
➤Occupation:Bus driver
➤Patient is married .
➤Patient takes mixed diet and has a decreased appetite .
➤Sleep : Regular
➤Bowel movements are regular and bladder movements are reduced .
➤Consumes 600ml alcohol occasionally and stopped 1 year back.
➤smokes beedi 1 pack per day and stopped 3 months back
GENERAL PHYSICAL EXAMINATION:
Patient is conscious ,coherent and cooperative and well oriented to time, place , person.
Patient was examined in a well lit room after taking their consent.
Patient is severely undernourished with marked sarcopenia
Pallor- present
Icterus -absent
Cyanosis-absent
Clubbing-absent
Generalised Lymphadenopathy-absent
Edema-bilateral pedal edema present
VITALS
➤Temperature : 98.3℉
➤PR : 90 beats per minute
➤BP : 100/70 mm of Hg
➤RR : 22 cycles per minute
➤SpO2 : 96% room air
SYSTEMIC EXAMINATION
Per abdomen -
Abdominal girth- 93-->91cm
Inspection-
Abdomen is distended , flanks are full, skin is stretched , no visible peristalsis , equal symmetrical movements in all quadrant’s with respiration
Palpation -
No local rise of temperature, no tenderness
All inspectory findings are confirmed by palpation, no rebound tenderness, gaurding and rigidity.
No tenderness , No organomegaly
Fluid thrill present
Percussion:
Shifting dullness present
Auscultation:
Bowel sounds heard
CVS : S1 and S2 heart sounds heard
CNS: No focal neurological deficits
Cranial nerves,motor and sensory functions intact.
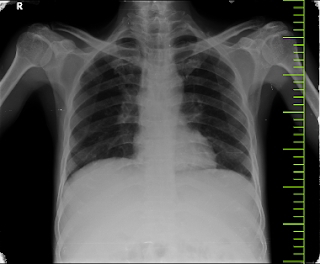
RR: BAE Present, normal vesicular breath sounds heard,no adventitious sounds
shape of the chest: normal
trachea appears to be central
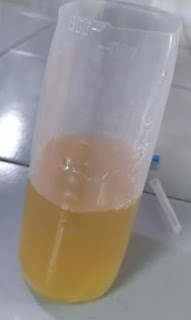
Ascitic fluid
PHES test
Interpretation :
INVESTIGATIONS
1. Complete Urine Examination
2. Anti-HCV Antibodies
3. GRBS
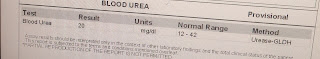
4. Blood urea level
5. HBsAg
6. Hemogram
7. HIV Rapid test
8. LFT
9. Serum Creatinine
10. APTT
11. Bleeding and clotting time
12. Prothrombin time
Ascitic tap -
Appearance - clear , yellow coloured
SAAG - 1.65 g/dl
Serum albumin - 2.0 g/dl
Asctic albumin - 0.35 g/dl
Ascitic fluid sugar - 104mg/dl
Ascitic fluid protein - 0.7 g/dl
Ascitic fluid amylase - 17 IU /L
LDH : 143 IU/L
Cell count- 50 cells
Lymphocytes nil
Neutrophils 100%.
TREATMENT :
Tab LASIX 40 mg PO BD
Syp. Lactulose 10 ml PO HS
Strict Alcohol abstinence .























Comments
Post a Comment