A CASE OF SLE PRESENTED IN OCTOBER 2023
NOTE:
- The following E-log aims at discussing our patient de-identified health data shared after taking the guardian's signed consent.
- Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve the patients clinical problem with current best evidence based input.
- This E-log also reflects my patient's centered online learning portfolio.
I have been given this case to solve in an attempt to understand the topic of "Patient Clinical Data Analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and providing treatment best to our skills and wisdom.
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitted.
A 25yr old female patient , presented to the casualty with complaints of fever and multiple skin lesions over both legs with suspected systemic lupus erythematous.
CHIEF COMPLAINTS
➤ Multiple skin lesions over both legs since 4 days .
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 6 years back . Then during her second pregnancy , she developed hyperpigmented lesion over her both cheek initially small in size which latter progressed to butterfly shaped lesion.
Since 3 months she is having high grade fever and went to rmp and used medication She also had abdominal pain for which she was admitted in our hospital on 26/8/23 and was treated as acute gastritis .
After discharge she developed skin lesions over b/l lower limbs associated with itching which later progressed to painful pus filled ulcers over b/l lower limbs ,over left elbow and lumbosacral region
Since 3 months she has complaints of hairfall and multiple joint pains i.e in elbow,wrist joint,interphalengeal joints and knee joint .
She had 2 episodes of generalized tonic seizures for about 2 minutes with uprolling of eyes , lip biting 5 days ago .
Not associated with involuntary micturition, defecation ,frothing.
No previous abortion history
Since 3 months she has ammenorrhoea.
Daily Routine : Before Disease - She used to wake up at 5 am then freshen up.
At 6am she used to do her household chores.
At 7am she used to have a cup of tea with her husband and then prepare both breakfast and lunch(she packs it to work) for herself and her family.
By 8 they leave her son at school and they both go to work.
At 2pm she used to have lunch at her workplace.
And by evening 4 they return home and after doing household chores she used to sleep by 9pm.
After Disease : No fixed time of getting up in the morning as she doesn't have to go for work.
Not doing any house hold chores.
She is mostly lying on bed.
She needs support from her husband for taking bath and changing dress.
HISTORY OF PAST ILLNESS
➤Not a K/c/o diabetes, hypertension, asthma , epilepsy tuberculosis , CAD
➤No surgical history
➤No history of Blood transfusions.
PERSONAL HISTORY
➤Occupation: Farmer.
➤Patient is married .
➤Patient takes mixed diet and has a normal appetite
➤Sleep : Regular
➤Bowel and bladder movements are regular
➤No known allergies and addictions.
FAMILY HISTORY
No similar complaints in other family members.
GENERAL EXAMINATION
➤Pallor : Seen
➤Icterus : Not seen
➤Cyanosis : Not seen
➤Clubbing : Not seen
➤Lymphadenopathy : Not seen
➤Edema : Not seen
VITALS
➤Temperature : 98.3℉
➤PR : 90 beats per minute
➤BP : 100/70 mm of Hg
➤RR : 20 cycles per minute
➤SpO2 : 96% in room air
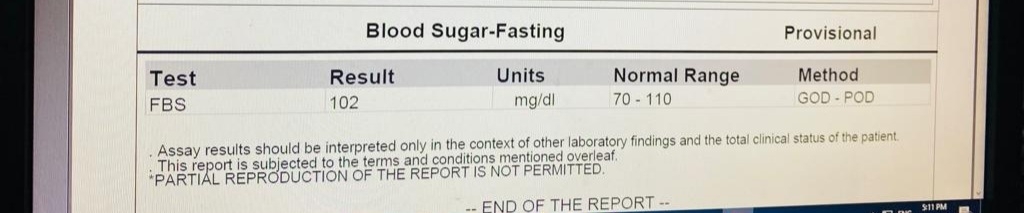
➤Blood Sugar (random) : 97mg/dl
SYSTEMIC EXAMINATION
CARDIOVASCULAR SYSTEM EXAMINATION
➤s1 and s2 heard
➤Thrills absent.,
➤No cardiac murmurs
RESPIRATORY SYSTEM
➤Normal vesicular breath sounds heard.
➤Bilateral air entry present
➤Trachea is in midline.
ABDOMINAL EXAMINATION
INSPECTION
➤Shape - Scaphoid
➤Equal movements in all the quadrants.
➤No visible pulsation, dilated veins and localized swellings.
PALPATION
➤Liver , spleen not palpable.
➤No tenderness
CENTRAL NERVOUS SYSTEM EXAMINATION
➤Conscious and coherent
➤Speech : Normal
➤No signs of meningeal irritation
PROVISIONAL DIAGNOSIS : Pyoderma gangrenosum secondary to SLE(?) associated with Anemia secondary to chronic inflammation and Hypotonic hyponatremia .
Clinical images
INVESTIGATIONS[11/10, 8:49 pm] Intern : LDH -200
Retic count -0.5
[11/10, 9:01 pm] Dr : Unnecessary tests
[11/10, 9:03 pm] Dr : Dermatology plan for this?
[11/10, 9:07 pm] Intern : Dermatology referal was taken and they also adviced to send ANA profile and also for biopsy sir
[11/10, 9:14 pm] Dr : Let's get the biopsy
How much will that cost?
Meanwhile let's begin her on tablet prednisolone 30 mg for suppressing the immune mediated inflammation
[11/10, 9:15 pm] Dr : We can MS Sir to make the biopsy free
[11/10, 9:15 pm] Dr : Also get 24 hour urine for protein and creatinine
[11/10, 9:15 pm] +91 Intern : Ok sir
[11/10, 9:16 pm] +91 Intern: Yes sir we r sending it tomorrow morning
[11/10, 10:44 pm] +Intern : Spot upcr 0.32
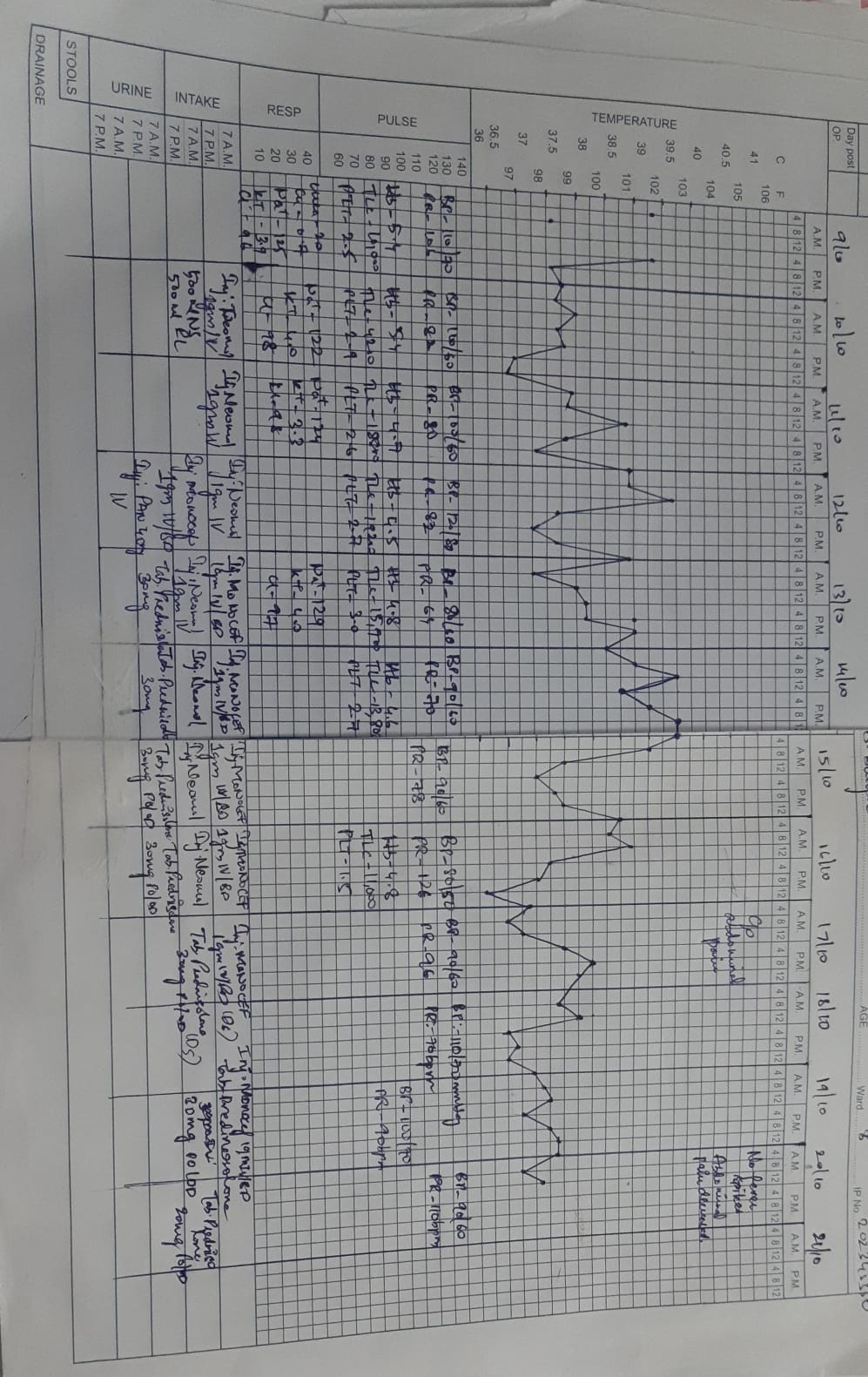
[12/10, 10:53 am] Dr : Fever chart update?
[12/10, 11:44 am] PG : Is just conservative medication enough for fevr sir
[12/10, 11:45 am] PG : Pulse rate 82, for such high temp ,relative bradycardia????
[12/10, 11:46 am] +91 Intern : Is the fever spike due to autoimmune etiology and the leucocytosis a reactive leucocytosis sir??
[12/10, 11:46 am] +91 PG : Any meningeal signs?
[12/10, 11:51 am] +91 Intern : Those are 8 am readings sir
Now her pulse rate is 100
Blood pressure is
110/60 mmhg sir
[12/10, 11:52 am] +91 PG : Cultures sent?
[12/10, 11:53 am] PG : Respiratory rate??
[12/10, 11:56 am] Intern : 24 cpm mam
[12/10, 11:56 am] PG : Sent sir
Waiting for reports sir
[12/10, 2:06 pm] Dr : Is systemic anti-inflammatory steroids conservative management?
[12/10, 2:06 pm] PG : Crp or esr?
[12/10, 2:08 pm] Dr : What are the chances of growing Salmonella or any other organisms (let's say such as those found in a systemic UTI) in this particular situation?
To me it appears less likely
[12/10, 2:09 pm] Dr : Why wouldn't they be elevated?
[12/10, 2:09 pm] Dr : Waste of money
[12/10, 2:09 pm] PG : Agree.
Just asked meningeal signs if there can be any source of new undocumented infection.
[12/10, 2:09 pm] Dr : 👆sepsis
[12/10, 2:09 pm] PG : Very well agree
[12/10, 2:10 pm] PG : In its absence,hoped if we can see crp or esr to try to get on to something else(abductive reasoning)
[12/10, 2:11 pm] Dr : We had a patient like her who also had meningoencephalitis (was presented in the Jan 25 OCC Nkp Cpd this year) @+91 97040 90596 Can share the link to that case report?
[12/10, 2:12 pm] PG : There's a similar case which me and another PG sr examined.
Unfortunately it was long lost with lack of digital traces(PaJR)
Hence asked about meningeal signs
[12/10, 2:13 pm] Dr : They are non specific inflammatory markers and she's already shouting inflammation
Currently we just need to cover for Salmonella treating monocef Deficiency along with 30 mg prednisolone suggested yesterday
[12/10, 2:13 pm] Dr : You are probably talking about the same patient. Nothing is lost except intern's memories
[12/10, 2:14 pm] PG : Very likely
[12/10, 2:14 pm] Dr : Please share the Dermatology notes asap
[12/10, 2:16 pm] Intern : Direct Coombs Test positive
[12/10, 2:26 pm] Dr : 👏👏Some placebo test finally to justify our steroids!
[12/10, 2:26 pm] Dr : Boundary 👏👏👏
[12/10, 2:29 pm] Dr : Currently we just need to cover for Salmonella treating monocef Deficiency along with 30 mg prednisolone suggested yesterday
[12/10, 7:53 pm] PG : https://www.nature.com/articles/s41598-022-05807-6
although there are many criteria for SLE diagnosis, all of them are classification criteria, rather than diagnostic criteria. That is, patients who even meet the criteria such as the SLICC classification criteria for a diagnosis of SLE are not necessarily SLE. Therefore, while taking advantage of high sensitivity of low titers of ANA to include suspected patients into diagnostic consideration, understanding specificity of high titers of ANA can help improve the accuracy of SLE diagnosis, reduce misdiagnosis and make clinicians more certain in SLE diagnosis, especially in complicated patients.
[12/10, 8:50 pm] Dr : 👏👏I take it that the article quote supports our stance not to get the dubious ELISA ANA costing 2,500!
[13/10, 9:28 am] PG : PR 64??
[13/10, 9:29 am] Intern : Yes ma'am
[13/10, 9:34 am] Dr : Parenteral antibiotics ceftriaxone asap
[13/10, 9:34 am] Dr : Share the entire hourly vitals chart here asap
[13/10, 9:35 am] PG : Okay sir
[13/10, 9:35 am] Intern : Ok sir
[13/10, 1:57 pm] UG student : https://asjad24.blogspot.com/2023/10/a-case-of-25f-presented-with-fever-and.html
[13/10, 2:49 pm] Dr : Second patient or previous one?
[13/10, 2:50 pm] Dr : Ask student to present to you both the cases and see if he can present on 18th
[13/10, 3:53 pm] UG student: Sir second patient which is currently admitted in amc
[13/10, 4:08 pm] Dr : Present both of them to us tomorrow
[13/10, 4:08 pm] Dr : Today to PG
[13/10, 4:12 pm] UG student : Okay sir
[13/10, 4:16 pm] Dr : Hourly BP chart update?
Soap update?
[13/10, 9:03 pm] Dr : Today's treatment update?
[13/10, 9:34 pm] Intern : Inj. MONOCEF 1gm IV/BD
inj.PAN 40 IV/OD
[13/10, 10:52 pm] Dr : Steroids?
[13/10, 11:35 pm] PG : Do we attribute the recent temperature trends to 'infection of unknown/undocumented source' or due to sequelae of Lupus?
Can we address both?
We would like to me as minimal and precise as possible but when there's complexity,what may be the better approach?
Address both promptly?
However,polypharmacy,drug drug interactions based on genomics and phenotypes shall also be taken into account?
Nonetheless the most valuable intervention would be to stay with patient,make friends and just travel the journey with her and hope it self optimises itselves while we do our evaluation and etc
[13/10, 11:35 pm] PG : Very well agree and reasonable
[14/10, 12:17 am] PG : To be*
[14/10, 7:03 am] Dr : We have been trying to address both since last few days as the conversation trail may suggest if one can scroll up and read them but then I'm not yet sure if both have been implemented
[14/10, 8:57 am] PG : Thanksss
[14/10, 8:58 am] PG : @+91 95057 66290
Update SOAP
[14/10, 8:58 am] Intern : Fever chart
[14/10, 9:36 am] Dr : Please add the treatments!!!
[14/10, 9:38 am] Dr : Look at how discordant the Day 2 WBC counts are with the rest of her journey here .
Does this tell you something about the sampling universe of this patient's peripheral blood that may not always represent all it's deeper circulation?
[14/10, 9:51 am] PG : What about her hb sir ..should we correct it
[14/10, 9:57 am] PG : Add the treatment and reshare the chart
[14/10, 10:12 am] Dr : Did you add the treatment for her hemolytic anemia that we proposed few days ago. Without that whatever blood you give will be hemolyzed again
[14/10, 10:17 am] PG : Maam the casesheet is with the sister who went to take medicines
Treatment :
Inj.monocef 1gm iv
Inj . Neomol at 7am
[14/10, 10:20 am] PG : Yes sir added
[14/10, 10:25 am] Dr : 👆Doesn't seem to have been here?
When added?
[14/10, 11:02 am] Intern : Yesterday sir
[14/10, 12:48 pm] PG : Tab.prednisolone 30 mg given sir
[14/10, 2:54 pm] Dr : 👆Not mentioned here
Mention when monocef started and when Prednisolone started
[14/10, 10:54 pm] Dr : @+91 90106 51652 Your fever chart contained identifiers
[14/10, 10:55 pm] Intern : Sorry sir, I'll remove them and send
[15/10, 7:28 am] Dr : Thanks. Today's update? Didn't see her in the afternoon AmC yesterday!
[15/10, 7:52 am] Intern : She is in ward sir
[15/10, 8:01 am] Dr : Oh she was stable enough to be transferred there?!
Please share her BP chart since admission along with the intervention
[15/10, 8:24 am] PG : Yes sir she is stable
[15/10, 9:14 am] PG : Bp charting
[15/10, 11:04 am] Dr : The resident changed from American to British after 7 AM but the dates didn't
[15/10, 11:07 am] Dr : 👆please update this
[15/10, 11:07 am] Intern : Ok sir
[15/10, 12:08 pm] Dr. Rakesh Sir Kims: Thanks
[16/10, 8:25 am] Dr : Will be looking forward to your reviewing the clinical significance of all the anti nuclear antibodies mentioned in the above report done by 2,500 borne by a few medicine resident's out of pocket expenditure
[16/10, 8:26 am] Dr : [10/16, 7:22 AM] intern : Sir she also has ant wall hypokinesia ..so should we start her on antiplatelets sir
[10/16, 7:30 AM] Dr : Share the Echo video in the group
[10/16, 7:30 AM] Dr : How do antiplatelets act in coronary vasculitis?
[16/10, 8:27 am] Dr : 👆UG student
[16/10, 9:14 am] PG : Today’s soap update
[16/10, 9:20 am] : PG If u are in opd, ask ward intern to update the case
[16/10, 9:41 am] Dr : Please join the previous charts!! 🧐😳
Daily input output?
[16/10, 9:42 am] Dr : Daily hourly BP plotted from Day 1 ?
What was the reason for hypotension? Adrenal crisis?
[16/10, 2:30 pm] PG : Purpose: Systemic lupus erythematosus (SLE) is an autoimmune disease with multi-organ involvement. Hyponatremia is common in inflammatory diseases such as meningitis. Also, it has been found to be strongly associated with the degree of inflammation. However, it has not been fully evaluated in lupus. This study aimed to assess the inflammatory impact of hyponatremia in SLE patients and investigate its relationship with SLE disease activity.
Patients and methods: A total of 101 patients with SLE were enrolled in this study and divided into two groups according to Na level; a normo-natremic group and a hyponatremic group. Demographic and clinical data were collected. SLE activity was assessed by the systemic lupus erythematosus disease activity index (SLEDAI). The estimated sedimentation rate (ESR) as well as levels of C-reactive protein (CRP) and complements (C3 and C4) were measured.
Results: The majority of patients were females (98 subjects) (97%) with a mean age of 33±8 years. Out of 101 participants, 40 patients (39.6%) were hyponatremic with a mean Na level of 131.58±3.11 mmol/L. There was a statistically negative correlation between both ESR and SLEADI score and Na level (r=-0.436 and -0.436, respectively) with p=0.002, whereas Na level was positively correlated with complements, Cl, and albumin levels (r=0.653, 0.314, and 0.460, respectively) (p=0.000, 0.027, and >0.001, respectively). CRP was not correlated with Na level. ESR was independently correlated with hyponatremia at the 95% CI for Exp B (0.997-0.058) with a p-value of 0.048.
Conclusion: Hyponatremia could be used as an indicator of SLE activity. Also, it might be an easily and rapidly detected as well as a prognostically useful marker of inflammation.
https://pubmed.ncbi.nlm.nih.gov/32210647/
[16/10, 2:30 pm] +91 83176 69334: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7075429/
[16/10, 2:40 pm] Dr. Rakesh Sir Kims: Na d1 125,
D2 122
D3 124
D4 ?
D5 129
D6 ?
D7 ?
D8 ?
D9 ?
[16/10, 2:42 pm] Dr : Does this patient lack inflammatory markers!?
Please share the priority problem list for her and explain what has been done to address that!!
[16/10, 5:32 pm] PG : We didn't repeat the electrolytes daily sir ..as she is having hyponatremia since one month when she was admitted under surgery department
[16/10, 9:32 pm] Dr : What's the reason for her hyponatremia? Inflammatory? What are the pathways?
[16/10, 9:33 pm] Dr : 👆
[16/10, 9:44 pm] PG : Clinical Significance
Systemic autoimmune disorders affect 3-5% of the general population, and ANAs are one of the few specific disease markers in their diagnosis.
Therefore, ANA testing is often the first step in diagnosing systemic autoimmune connective tissue disorders. Laboratories report the staining pattern and the titer of ANA as an indication for further testing. The presence of ANAs and their subtypes increase the likelihood of a systemic autoimmune disorder, and there are notable clinical correlations between the ANA subtypes and autoimmune connective tissue disorders. However, they do not necessarily confirm that an individual has or will develop an autoimmune disease. Although positive ANA results help diagnose several autoimmune disorders, the negative ANA titer is also expected in some specific inflammatory conditions, for instance, ankylosing spondylitis.
Systemic Lupus Erythematosus (SLE)
Systemic Lupus Erythematosus (SLE) is a chronic autoimmune disorder that affects nearly every system in the body. Individuals have variations in disease presentation, where one system often deteriorates significantly more than the others. Clinical manifestations may include fatigue, arthritis, vasculitis, nephritis, pleuritis, and myocarditis. Clinical manifestations and immunologic criteria are required to establish a definitive diagnosis of SLE. Immunologic criteria include abnormal ANA titers in the absence of drugs and the presence of anti-dsDNA or anti-Sm antibodies.
https://www.ncbi.nlm.nih.gov/books/NBK537071/#:~:text=Clinical%20Significance&text=%5B22%5D%20ANA%20testing%20has%20long,arthritis%20compared%20to%20healthy%20controls.
[16/10, 9:47 pm] PG : patients with profile A (anti-nDNA and/or anti-Sm antibodies) had a statistically significant increase in malar rash, renal and hematologic involvement and hypocomplementemia when compared to patients with a negative profile. Patients with profile B (anti-nRNP antibodies) had a clinical pattern of disease different from that of patients with profile A and had a statistically significant increase in Raynaud's phenomenon when compared to patients with a negative profile. Patients with profile C (anti-SSA and/or anti-SSB antibodies) had a statistically significant increase in lupus-related rashes and photosensitivity. None of the lupus patients reviewed in this study has profile D (antibodies to centromere and/or Scl-70), this profile being seen largely in patients with scleroderma or one of its variants. Both patients with profile E (anti-histone antibodies) had drug-induced lupus.
[16/10, 9:47 pm] Intern : https://pubmed.ncbi.nlm.nih.gov/8485555/
[16/10, 9:49 pm] Intern : Sensitivity And specificity of antibodies
[16/10, 9:50 pm] Intern : https://pubmed.ncbi.nlm.nih.gov/19854810/
[16/10, 10:07 pm] Dr : 👏👏
[16/10, 10:08 pm] Dr : Which one among these in our patient?
[16/10, 10:09 pm] Dr : Our patient has profile C.
Any other articles correlating this with the kind of findings our patient has?
[17/10, 7:08 am] Dr : What was the gold standard comparator while testing for sensitivity and specificity of ANA? Clinical findings?
[17/10, 10:42 am] Intern : Sir this is with regard to lupus nephritis
Where gold standard is taken as biopsy proven cases sir
[17/10, 10:47 am] Dr : And what were the gold standard findings of those biopsies?
[18/10, 8:31 am] Dr : Please join both the fever charts and then share asap
[18/10, 8:33 am] Dr : Now that we gave her treatment for both typhoid and SĹE did the fever come down due to treatment of typhoid or SLE?
[18/10, 8:38 am] Intern : Treatment of SLE sir
[18/10, 8:40 am] Dr : PG Use this one for your presentation today
Please video it and share the YouTube link here
[18/10, 8:40 am] Dr : Coin toss?
[18/10, 9:09 am] PG : Why can’t it be typhoid which ressolved
[18/10, 9:10 am] Dr : How's the patient subjectively?
[18/10, 9:12 am] PG : Subjectively she is better sir
[18/10, 9:16 am] PG : Update in soap format
[18/10, 9:20 am] Dr : In the fever chart. Enter the missing subjectivities in the daywise slots there since admission
[18/10, 10:16 am] Intern : Her fever spikes came down after giving her prednisolone mam
[18/10, 10:22 am] PG : What does prednisolone do
[18/10, 10:29 am] Dr : Monocef was also given at the same time?
[18/10, 3:49 pm] Dr : Overtesting because of unclear ultrasound report!!?
[18/10, 4:05 pm] PG : Urology sir adviced it to rule out any distal ureteric calculus sir
[18/10, 4:08 pm] Dr : Done?
[18/10, 4:09 pm] Dr : How many X-rays equal one CT scan in terms of radiation?
[18/10, 4:09 pm] PG : I have the video sir
I should upload it in youtube channel sir
Im doing it sir
[18/10, 4:10 pm] Dr : The patient is ours. We need to decide if the investigation is useful or not
[18/10, 4:42 pm] Dr : 100-800 chest x-rays.
https://www.epa.gov/radiation/how-much-radiation-am-i-exposed-when-i-have-ct-scan
[18/10, 4:42 pm] PG : 70-100 X rays equals 1 CT sir
Each X ray has 0.1msv
While each CT 7msv
[18/10, 4:43 pm] Dr : Chest X-ray 0.02 mSv
Abdominal CT 10 MSv
[18/10, 5:01 pm] PG : https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8848057/
Moreover, early HCQ use in antinuclear antibodies positive individuals might delay the progression to SLE. Finally, HCQ has a significant favorable impact on long-term outcomes such as damage accrual and mortality in SLE. Based on these multiple benefits, HCQ is now the mainstay long-term treatment in SLE,
[18/10, 5:42 pm] Intern : .
WHO classification based of histopathology
Class 1 - Minimal Mesangial Lupus Nephritis
Light microscopy findings - Normal
Immunofluorescence electron microscopy findings - Mesangial immune deposit
Class 2 - Mesangial Proliferative Lupus Nephritis
Light microscopy findings - Mesangial hypercellularity purely or expansion of mesangial matrix with mesangial immune deposits
Immunofluorescence electron microscopy findings - Mesangial immune deposits with few immune deposits in subepithelial or subendothelial spaces possible
Class 3 - Focal Lupus Nephritis
Light microscopy findings - Active or inactive with focal, segmental, or global involvement affecting fewer than 50% of all glomeruli
Immunofluorescence electron microscopy findings - Mesangial and subendothelial immune deposits
Class 4 - Diffuse Lupus Nephritis
Light microscopy findings - Active or inactive with diffuse, segmental, or global involvement affecting approximately 50% of all glomeruli. It is subdivided into diffuse segmental (class 4-S) when around 50% of involved glomeruli manifest segmental lesions (meaning less than half of glomerular tuft is affected) and diffuse global (class 4-G) when approximately 50% of affected glomeruli have global lesions. It shows wire-looping.
Immunofluorescence electron microscopy findings - Subendothelial immune deposits
Class 5 - Membranous Lupus Nephritis
Light microscopy findings - Diffusely thickened glomerular basement membrane with no inflammatory infiltrate. It can possibly show subepithelial deposits and basement membrane spikes on specific stains, such as silver and trichrome. It may occur in combination with class 2 or 4 and may reveal advanced sclerosis.
Immunofluorescence electron microscopy findings - Subepithelial and intramembranous immune deposits.
Class 6 - Advanced Sclerosis Lupus Nephritis
Light microscopy findings - Advanced glomerular sclerosis affecting almost 90% of glomeruli, tubular atrophy, and interstitial fibrosis, all manifestations of irreversible renal injury
[18/10, 5:43 pm] PG : Though the article did not say regarding the biopsy findings in their cases sir
But was mentioned regarding WHO class 3,4,5 ...
[18/10, 5:43 pm] PG : https://www.ncbi.nlm.nih.gov/books/NBK499817/
[18/10, 5:43 pm] PG : https://youtu.be/O3gLw_UuEoM?si=8z-xgKd50qkMxixf
[18/10, 6:25 pm] Dr : Share the scientific evidence in a PICO format instead of opinion?
[18/10, 6:26 pm] Dr : What is specific to Lupus about these histopathology findings? Can't they be seen in any of the similarly classified primary glomerulopathies?
[18/10, 6:28 pm] Dr : Check again. Perhaps the gold standard criteria was clinical?
[18/10, 8:06 pm] Dr : Please upload all the above PaJR conversations and images and links into your case report in the same timelined sequence
[18/10, 8:08 pm] UG student: Okay sir
[19/10, 9:13 am] Dr : Is she still on 30 mg of prednisolone?
[19/10, 9:22 am] PG : Yes sir
[19/10, 9:31 am] PG ; Will make it 20mg today sir
[19/10, 9:44 am] Dr : Share the psychiatry notes
[19/10, 9:54 am] Dr : Always check if the AM PM lines are matching properly while joining the charts
[19/10, 10:03 am] PG : Okay sir
[20/10, 9:29 am] Dr : Thanks!
AsK everyone else to share their cases in this manner
[20/10, 10:08 am ] PG : Okay sir
[24/10, 10:15 am] Dr : Please upload and update this and the other information here to the case report asap.
[24/10, 10:27 am] UG student : Okay sir




















Comments
Post a Comment